Palliative care is meant to provide comfort, but the facts are quite different. Numerous families experience absolute clarity when confronting the matter, only to leave with confusion and even a feeling of being deceived. This article explores the reasons behind people’s negative perception of palliative care and the continuous failure of the system to address the issue.
Why Palliative Care Is Bad (based on the frustrations that people express)
People hardly dare to talk about palliative care. The truth is that palliative care is seen by some as highly compassionate, while others interpret it as the point when hope is quietly taken away from the room. So that’s exactly the tension close relatives rant about on the web after their experience. It is not the concept which is wrong, but the manner in which it is delivered, explained, timed, or in most cases, given without enough background.
Not a medical verdict. This is the side of life which is messy and gets ignored.
Palliative palliative — the repetition that shows confusion in the system
Indeed, people say “palliative palliative” when they are confused. It appears in their notes, in brief talks, as if by repeating the word they could finally grasp its sense. But that is the problem: palliative care is hardly ever explained in detail.
Most families recall that day like it was yesterday:
A doctor comes in, heaves “palliative care” at them, and just leaves them there — emotionally empty. No gentle approach. No real explanation. Just a new tag thrown at their lives.
And then they look it up on the internet. That’s when the terror takes over.
Hospice and palliative care meaning (and why many think it’s bad)

Much of the irritation arises from the confusion between hospice and palliative care. Even some professionals occasionally confuse the two.
| Term | Real Definition | Why Families Feel Misled |
| Hospice | Care for people very close to death, normally when curative treatment is stopped. | Feels like “giving up,” although that is not the intention. |
| Palliative Care | Support for symptoms during a serious disease, at any stage. | Often introduced only very late, so it is mistaken for hospice. |
When people ask what palliative care is, they are often given a sugar-coated version: “We help with comfort.” But comfort is too general. Comfort is not a plan. Comfort does not explain the change of mood from aggressiveness in treatment to something gentler and frightening.
And yes… just this one misunderstanding is responsible for a huge number of online discussions, where the question “why palliative care is bad” is raised, is fuelled.
Define palliative medicine (without the glossy brochure tone)
So, from a technical point of view, palliative medicine is based on symptom reduction, quality of life improvement, and care coordination.
However, this neat definition rarely corresponds with reality. People say:
- It seems like the time is too short.
- It feels as if the decision-makers are talking about us, the family, while nobody is involving us.
- They give you the feeling that you should “come to terms with the inevitable.”
When navigating the complexities of advanced illness management, individuals often find themselves in a digital labyrinth. Searching for answers on the internet at such a time can be an isolating experience; the person searching is likely already deeply stressed and overwhelmed by the gravity of their situation.
Unfortunately, the solutions they encounter frequently focus on clinical logistics or administrative hurdles, rarely providing the comprehensive emotional support framework that patients and their families truly need. For those in Australia, navigating the intersection of medical care and financial stability is a significant part of this burden. Understanding the nuances of health insurance in Australia can help alleviate some of the peripheral stress, allowing families to focus more on the emotional well-being of their loved ones rather than just the rising costs of care.
By integrating practical resources like Australian health coverage with compassionate care models, we can begin to bridge the gap between clinical management and the human need for empathy and support during life’s most difficult transitions.
So yes, there is quite a big gap between theory and practice in this case.
Palliative services definition — and the gap between theory and what happens
Here’s the part that most people would rather not acknowledge.
The teams providing palliative services are very often short of staff, burdened with too much work, or weirdly separated from the doctors who look after the patients. The relatives have to tell their story over and over again to different people.
It is not “bad care”.
It is a bad system.
“Why didn’t anyone tell us earlier?”
“Why does every doctor give a different timeline?”
“Who is it that handles my dad’s painkillers?”
These openings become emotional sinkholes.
The palliative unit — where reality hits too fast
The palliative unit is supposed to be the supporter. Calm. Maybe even grounding. Sometimes it is. Although, on other occasions, families portray it as the place where “everything happened abruptly.”
One day, the medical team advocates all the possible treatments. The following day, they change their direction. Tone changes. Intent changes. Hope changes.This sudden change is the main reason why many people take pallative care (yes, people misspell it—shows how rushed everything feels) for a quiet way to the end. Leaving the unit and asking “what happens when I die” is more existential than medical at that point. The people are worn out. They want straightforwardness, not euphemisms.
Why some people believe “palliative care is bad” — the raw reasons
Without putting too much polish on them, let’s just lay them out.
Timing is nearly always terrible
Completely late introduction. That barely leaves any time for families to get used to it.
Communication may seem like performing a robot
Too many medical terms. Not enough love. People feel that they are handled instead of being listened to.
It indicates “no more treatment” even if that is not the case
Branding issue that is ignored.
Emotionally, it is like being hit by a brick
The term palliative carries a psychological burden that nobody is prepared for.
Some providers may lack the necessary soft skills
Unpleasant truth: some professionals are not trained to have the kind of talks that palliative care requires.
The system isn’t built for nuances
Illnesses are not straight lines. But healthcare bureaucracy is.
End of life care — the reason why topic frightens families
End-of-life care is yet another term that is used very loosely in hospitals. But the families interpret it as something else:
- finality
- loss
- decisions they are not ready to make
When people say that “palliative care is bad,” they often mean:
“This was the last thing I expected, and nobody helped me to understand what was going on.”
The fact is that end-of-life care may be loving and supportive—but this is not the case when it is done in a hurry, whispered, or in a monotone during a 7-minute consultation.
The emotional clash: hope vs. acceptance
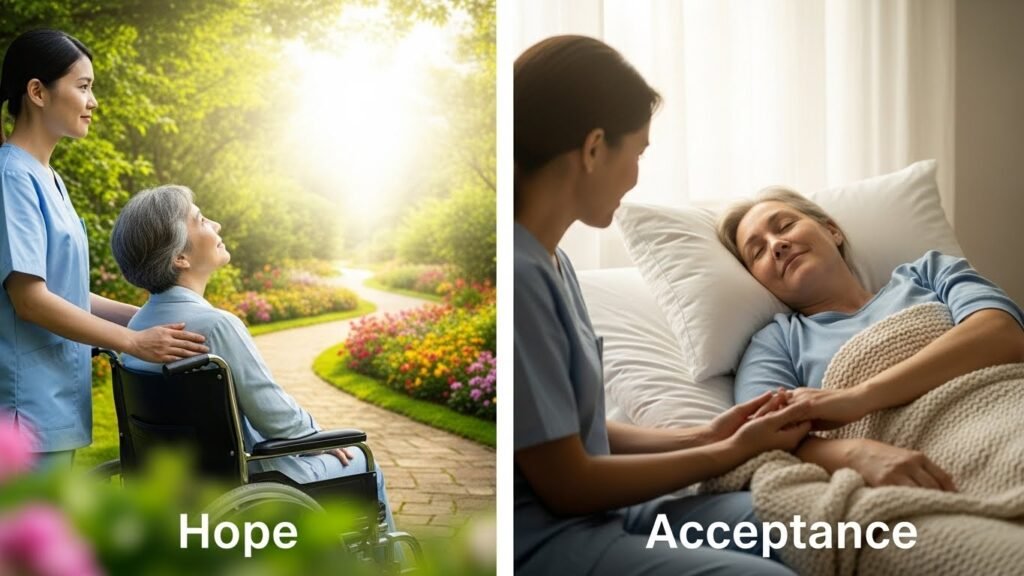
Some patients are still eager to have treatment. Some families hold on to hope. The palliative teams are sometimes accused of being too realistic, too soon.
It is not the care that causes harm.
It is the emotional mismatch.
The very mismatch causes the protagonists to harbor resentment… and thus they make internet postings about palliative care being cold, harsh, or insensitive.
Random but requested integration — cybertruck price in pakistan
People put the strangest things into the search engine when they’re in a crisis. Grief makes your mind jump from one thing to another — e.g., while waiting for the news about a loved one you can be looking for the cybertruck price in Pakistan. Strange but true.
The same randomness is there in the processing of palliative transition by the families.
(That’s twice. One more later.)
The lived experiences people repeat online
“They talked over us.”
Communication hierarchy. It’s a thing.
“We didn’t understand the medications.”
The explanation of how to manage pain in simple terms is missing from the package.
“Everything changed overnight.”
One hospital meeting can change the whole plan.
“It felt like they’d given up on my parent.”
Even when that wasn’t the case.
The financial side nobody explains upfront
Matter of money isn’t always on the people’s lips, however, it is there—making the care decisions slowly but surely. And in places where medical systems are not properly financed, the families are left with figuring out the cost of palliative services, insurance coverage, and what is the part that should be paid out-of-pocket.
Truth be told, it is anxiety-provoking at the worst time possible. Like looking for the cybertruck price in Pakistan when you are trying to take your mind off too many overwhelming bills.
(That’s the third time.)
So… is palliative care bad? Or is the system broken?
The system. Almost always the system. The care intention of palliative care is positive. Even great.
But intentions are of no use when there is no communication. Or when the timing causes traumas. Or when the families are taken aback by medical jargon they have never come across before.
It is from here that the whole “why palliative care is bad” story originates — a mix of or rather an intersection of — unfulfilled expectations and raw emotions.
And it doesn’t go away.
5 FAQs (things “People Also Ask” about palliative care)
- Is palliative care the same as hospice?
Not really, however, people confuse them all the time. Hospice is for end-of-life care, while palliative care can be started any time during an illness. - Does palliative care mean a patient is dying soon?
Not at all. Most of the time, it is introduced very late, thus the patients’ relatives infer this, but that is not the case. - Why do families feel upset when palliative care is suggested?
It happens that the presentation is abrupt, without any emotional support, and gives the impression of a detachment from the active treatment. - Who decides when palliative care begins?
Generally doctors, but in an ideal world, it should be a decision made by the patient and family. Unfortunately, in reality, there are gaps in communication which make it unclear. - Can patients leave palliative care and come back to curative treatment?
Absolutely. A palliative care plan is not an obstacle to other treatments, though a lot of people are under the wrong impression.